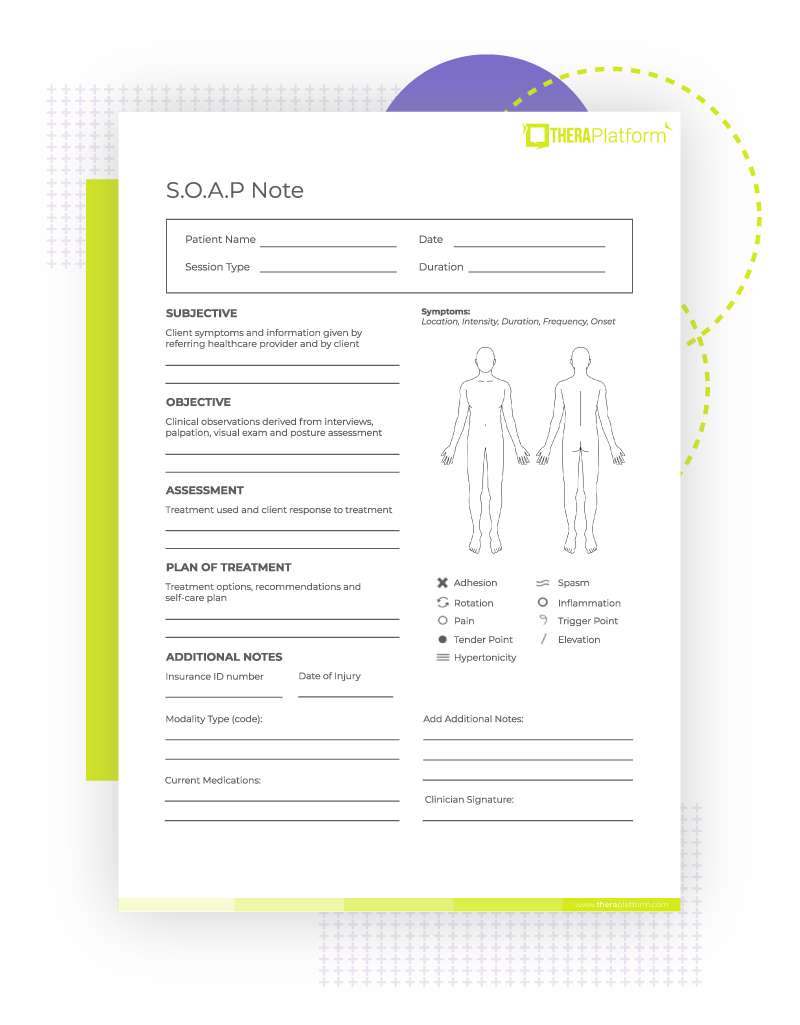
Soap Notes Physiotherapy Template
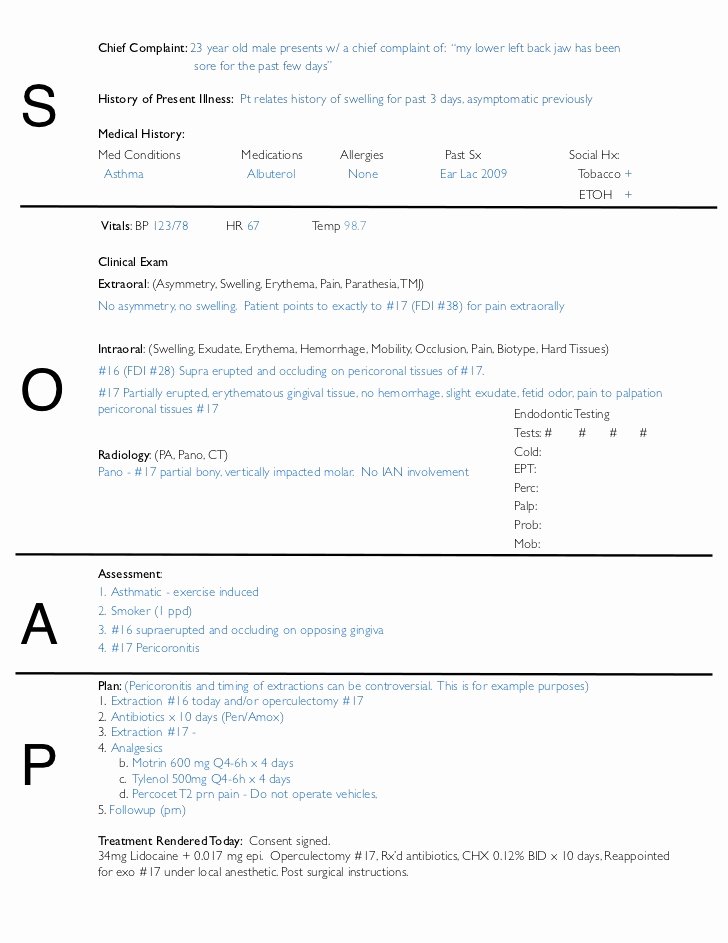
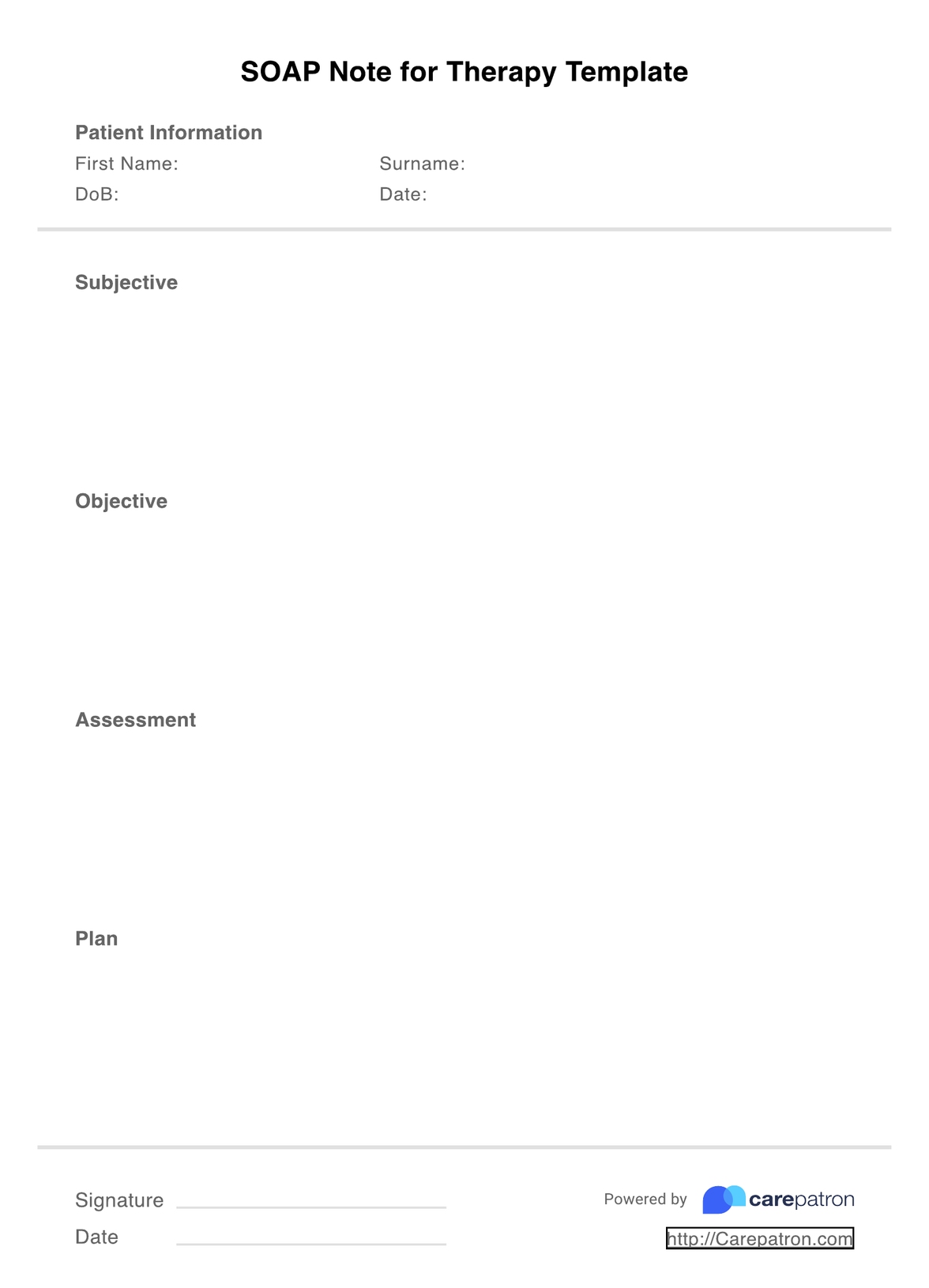
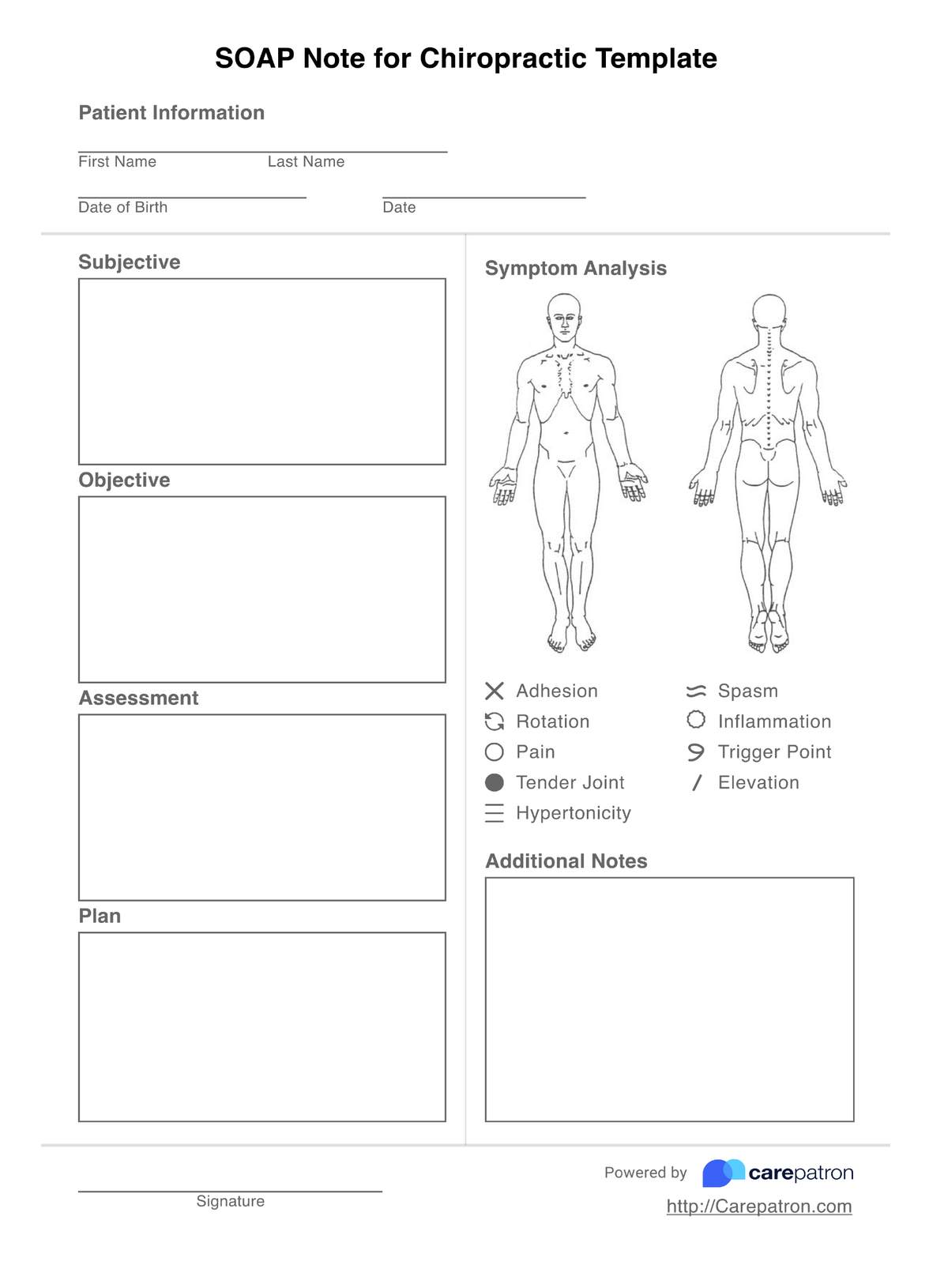
Soap Notes Physiotherapy Template - Use this free physical therapy soap note template during patient sessions to effectively capture subjective and objective data. Soap notes are a methodical way to document each visit, broken into four parts: The patient’s personal report (subjective), what is observed and measured (objective), the. Our free, downloadable physical therapy soap note template includes examples of each section including subjective, objective, assessment, and plan. The patient reports sudden onset of lower back pain after lifting a heavy box two days ago. Here’s a revised—and more detailed—example of the note. The soap format can be one of the most effective ways for clinicians to document and objectively assess,. Soap notes are a standardized form of note taking that can serve as evidence of patient contact and effectively communicate important information to the entire care team. The acronym stands for subjective, objective,. Here are some templates for writing soap notes. Soap notes are a methodical way to document each visit, broken into four parts: Soap notes are a standardized form of note taking that can serve as evidence of patient contact and effectively communicate important information to the entire care team. There's a pdf and a docx (word document) version. The soap format can be one of the most effective ways for clinicians to document and objectively assess,. But instead of downloading one. Download our free soap note template. pt assessment example with soap note when creating physical therapy assessment notes, utilizing a structured template can enhance clarity and consistency. They are commonly used by mental health professionals such as. Integration with client records and appointment schedules. Use this free physical therapy soap note template during patient sessions to effectively capture subjective and objective data. How do you write a soap note for physical therapy? Wondering how to write soap notes? The patient’s personal report (subjective), what is observed and measured (objective), the. There's a pdf and a docx (word document) version. Start with 3 free soap notes. The best way to write effective and reliable soap notes is to use a template, either created by yourself or using one. Start with 3 free soap notes. This guide provides detailed instructions for each section of a soap note, helping you understand. But instead of downloading one. Streamline the process of recording a patient’s physical treatment progress and plan. Download our free soap note template. The soap format can be one of the most effective ways for clinicians to document and objectively assess,. Integration with client records and appointment schedules. Here’s a revised—and more detailed—example of the note. Streamline the process of recording a patient’s physical treatment progress and plan of care using downloadable physical therapy soap note templates. Start with 3 free soap notes. Dap notes are progress notes used to document therapy sessions and track the progress of a treatment process. There's a pdf and a docx (word document) version. Soap notes are a standardized form of note taking that can serve as evidence of patient contact and effectively communicate important information to the entire care team.. pt assessment example with soap note when creating physical therapy assessment notes, utilizing a structured template can enhance clarity and consistency. Download our free soap note template. They are commonly used by mental health professionals such as. How do you write a soap note for physical therapy? The patient’s personal report (subjective), what is observed and measured (objective), the. Streamline the process of recording a patient’s physical treatment progress and plan of care using downloadable physical therapy soap note templates. Integration with client records and appointment schedules. The acronym stands for subjective, objective,. Download our free soap note template. Use this free physical therapy soap note template during patient sessions to effectively capture subjective and objective data. Here are some templates for writing soap notes. Streamline the process of recording a patient’s physical treatment progress and plan of care using downloadable physical therapy soap note templates. Soap notes are a standardized form of note taking that can serve as evidence of patient contact and effectively communicate important information to the entire care team. Soap notes are essential. Our free, downloadable physical therapy soap note template includes examples of each section including subjective, objective, assessment, and plan. Integration with client records and appointment schedules. There's a pdf and a docx (word document) version. Start with 3 free soap notes. Soap notes are a methodical way to document each visit, broken into four parts: They are commonly used by mental health professionals such as. Soap notes are a methodical way to document each visit, broken into four parts: Dap notes are progress notes used to document therapy sessions and track the progress of a treatment process. But instead of downloading one. Soap notes are essential for effective patient care and documentation in physical therapy. But instead of downloading one. Soap notes are a methodical way to document each visit, broken into four parts: How do you write a soap note for physical therapy? Some simple templates for the soap note format. Use this therapy note template to guide your daily note documentation. How do you write a soap note for physical therapy? Wondering how to write soap notes? This guide provides detailed instructions for each section of a soap note, helping you understand. Use this free physical therapy soap note template during patient sessions to effectively capture subjective and objective data. Soap notes are a standardized form of note taking that can serve as evidence of patient contact and effectively communicate important information to the entire care team. They are commonly used by mental health professionals such as. Use this therapy note template to guide your daily note documentation. Integration with client records and appointment schedules. Soap notes are a methodical way to document each visit, broken into four parts: Here are some templates for writing soap notes. Start with 3 free soap notes. Here’s a revised—and more detailed—example of the note. The best way to write effective and reliable soap notes is to use a template, either created by yourself or using one. pt assessment example with soap note when creating physical therapy assessment notes, utilizing a structured template can enhance clarity and consistency. But instead of downloading one. Soap notes are essential for effective patient care and documentation in physical therapy.SOAP Notes for Therapy Template & Example Free PDF Download
Free Physical Therapy SOAP Note PDF SafetyCulture
SOAP Note for Physiotherapy Assessment .pdf
Physical therapy soap Notes Template Shooters Journal
Soap Note Template 9+ Free Word, PDF Format Download!
SOAP Notes For Physical Therapy Template & Example Free PDF Download
SOAP Notes For Physical Therapy Template & Example Free PDF Download
SOAP Notes For Physical Therapy Template & Example Free PDF Download
Physical Therapy SOAP Note Interactive PDF Template
Physical Therapy Soap Note For Stroke Patient Minnesota Health Care
Streamline The Process Of Recording A Patient’s Physical Treatment Progress And Plan Of Care Using Downloadable Physical Therapy Soap Note Templates.
The Soap Format Can Be One Of The Most Effective Ways For Clinicians To Document And Objectively Assess,.
A Soap Note Template Is A Structured Method For Documenting Patient Encounters, Commonly Used In Medical Settings.
Dap Notes Are Progress Notes Used To Document Therapy Sessions And Track The Progress Of A Treatment Process.
Related Post:
.png)



.png)